HBOT is a most useful adjunct to the repair of broken or diseased bones and is helpful in the maintenance of bone health.
Bones – repair and good health
In order to understand why HBOT can assist, a simple explanation of bone growth and bone health is needed as a primer.
Bone cells can modulate (ie change to and from) into osteocytes, osteoblast or osteoclasts, depending on the stimulation or challenge that is presented to the body. For example, parathyroid hormone, electricity, weight bearing (exercise), diet, illness, or age cause bone to be in a continual state of dynamic flux within the body. An exchange of minerals is constant between the bone’s matrix, interstitial fluid and plasma. The flip-flop changes in bone-cells are normal and as the osteoclasts chew away at bone, it stimulates the osteoblasts to concrete that area with fresh hard bone.
Increased or decreased oxygen tensions also stimulates dynamic and significant changes in bone either to the patient’s benefit or detriment.
Animal studies have demonstrated that osteoclasts and osteoblasts (bone repair and maintenance cells) are exquisitely reactive to increased oxygen tensions. For example, higher treatment pressures excite bone cells to become the giant osteoclasts that give off a bone dissolving acid or chelate minerals from hard bone causing it to soften. Lower HBOT pressures stimulate the bone cells to become osteoblasts, forming new bone and concreting fractures together.
The bone cell reaction to treatment pressures may explain why some experimental animal studies on the effect of HBOT in orthopedics stand at odds with the others.
The clinical experience has been extremely positive. It must be emphasized that the “tweaking” of treatment pressures (intermittent changes between deeper and shallower on subsequent days) is always under the supervision of an orthopedic specialist.
Patient ‘Amci’, age nine
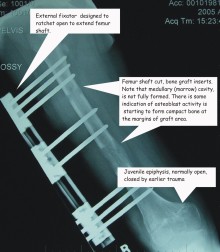
At the age of five, Amci was run-over by a car and sustained life-threatening injuries, including a crush injury to her right-hand thigh along with multiple fractures. Due to the crushing of the lower portion of her femur, the epiphyseal plate closed. A brief explanation will assist understanding of the sequels to Amci over the next four-year period and the challenge faced by the pediatric orthopedic surgeon who was trying to assist her.
Click medical images for a larger view
The ends of long bones are essentially spongy, surrounded by a thin layer of compact bone. To allow growth of the shaft, a juvenile has what is known as the epiphyseal plate, a thin layer of cartilage which is essentially the growth zone. As the juvenile approached adulthood, this cartilage hardens and this growth zone disappears.The crush injury caused Amci’s injured femur to stop growing. The result was that her uninjured leg was now much longer and Amci was lopsided. With the growth spurt of puberty approaching, five years after the accident, the strategy for a near normal life for her was surgery.
The now solid short femur was cut in two places and grafts placed as spacers. An external extender was attached to stabilize the bone. Each day, the extender placed additional tension on the femur. To slow the growth of the uninjured leg, the epiphysis was surgically modified.
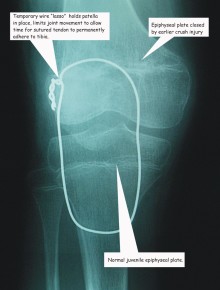
In an unfortunate complication the tendon that ran beneath Amci’s knee (patella) parted company at the tibial attachment point. Emergency surgery was performed, the tendon was sutured back in place, and to avoid it tearing before tensile strength glued the tendon to the bone, a wire support was inserted.
Problems
Now the problems set in. Not only was the femur unstable, the large surgical incision refused to close over and became infected. The Childrens’ Hospital orthopedic surgeon tried to find a hospital-based HBOT department to assist in Amci’s care with hyperbaric oxygen to close the surgical wound. All declined to do so.
Two days prior to the scheduled amputation of her leg, her surgeon found our clinic and Amci was discharged for treatments at HCA under the oversight of our orthopedic specialist.
Because of the immediate problem of the non-healing wound, Dr. Anderson recommended wound-care treatments of 48 fsw to reduce inflammation and swelling and to assist in killing the staphylococcus infection. However, in view of the underlying problem of slow bone growth in Amci’s femur with stimulated osteoclast activities possibly slowing progress, every five days the daily treatment pressure was reduced much lower in order to stimulate osteoblastic bone growth. Then, for the next five days, the treatment pressure went back to the wound-care protocol.
In addition to HBOT, Dr. Grady altered Amci’s nutritional intake to include nutraceuticals (mannatech.com) and also the drinking of unpasteurized (raw) milk. This was to ensure fast calcium and vitamin D intake to provide cellular support to the HBOT. Dr. Anderson also prescribed the use of electro-pulse (neromodulation) at the wound site to serve the dual purpose of eliminating the pain at the wound-site and stimulating the repair cells to produce adenosine triphosphate (ATP), energy fuel for new cell production.
Results
With seventy daily consecutive HBOT treatments, both Amci’s bone and skin healed in parallel rather than sequentially. The external fixator was removed and Amci is now acting as a high spirited little girl, skipping and playing. Amci’s future is bright because of the combination of disciplined medical skills of both orthopedic surgeons plus adjunctive HBOT. Amci was able to avoid amputation.
Amsi’s mother, Rosa has written about her little girl and Amsi’s courage and the help of family, friends and specialist physicians.
For that story, click Amci’s Story