Is that all there is to a Fire? Acute Smoke Inhalation
Prolonged exposure to unhealthy air can lead to respiratory, vision and large amounts of invisible carbon monoxide, a cellular poison is often present and can be measured in the patients blood as carboxyhemoglobin (COHb).
Pyrolysis – the chemical decomposition of organic materials by heating, e.g., burning carpets, plastics, etc – produce invisible and deadly poisons such as cyanide which can effect and even kill the stricken patient.
California’s wildfires exposed millions of persons to high levels of smoke inhalation. Firefighters, police officers and members of the public spent many hours exposed to the thick smoke. Hundreds were treated for “smoke inhalation problems.” Many of the elderly evacuees were taken to local hospitals with breathing problems.
A DOCTOR SHOULD BE CONSULTED WHENEVER THICK SMOKE IS INHALED FOR MORE THAN A FEW MINUTES OR WHENEVER THE FUMES ARE THOUGHT TO CONTAIN TOXIC SUBSTANCES.
Hyperbaric oxygen therapy (100% oxygen at 3 ATA) should be administered when carbon monoxide intoxication or cyanide poisoning causes loss of consciousness, altered mental state, cardiovascular dysfunction, pulmonary edema, and sever neurological damage.
OXYGEN UNDER PRESSURE BECOMES AN ANTAGONIST TO THESE CELLULAR TOXINS AND WILL DRIVE THEM FROM THE BODY.
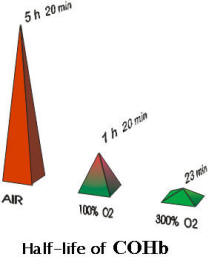
The graph clearly shows that when oxygen is administered in a HBOT chamber (the 300% pyramid), the half life of carboxyhemoglobin drops from over five hours in air to a little more than 20 minutes.
After the smoke clears . . . Is The Worst Over?
Usually not. The smoke and toxins, blown a thousand miles into the Pacific by the prevailing wind will return to land when the wind changes to an offshore flow. Headaches, runny noses and red-eyes will testify to the persistence of the event. Then, after all of the fires are extinguished, winds will blow up huge ash storms to torment the population. However, many persons who breathed the smoke will suffer serious and ongoing complications from the event.
The Chronic or Delayed Sequel and Occult (hidden) Carbon Monoxide Poisoning
Carbon Monoxide (“CO”) poisoning is one of the fourteen (UHMS) “approved” and reimbursable maladies that hospitals will treat in the hyperbaric chambers. However, most hospital based HBOT physicians will only treat the acute patient and expect a spontaneous resolution of symptoms. Nonetheless, there is a large amount of scientific literature that indicates that up to a year after exposure, patients can still suffer from the poisoning event and that HBOT can be used to return them to normal status.
“Misdiagnosing CO poisoning is common in the initial evaluation and management of the CO. Other diagnostic considerations include psychiatric illness, migraine headaches, stroke, acute alcohol intoxication, heart disease, flu, or even food poisoning. . . . Chronic symptoms may present as flu-like illness, headaches, tearfulness, depression, agitation, anxiety, decreased memory, attentional and concentration skills, poor reasoning skills, irritability, euphoria, and overall personality changes. Fatigue, headaches and dizziness are the three most common symptoms.” [1]
If you or your loved one have any of these symptoms, even months after “smoke Inhalation,” then you must consult a specialist physician. The diagnosis is complex but the treatment is simple — HBOT. To assist you and your physician, we will email you the excellent four page medical descriptions of this confusing ailment “Carbon Monoxide: Identification of Delayed Sequelae and Occult Exposure” — J. Thomas Millington, M.D. Joel Ellenswig, M.D. Karen L Shiltz, PHD — click here Make sure you include your request for this material in your email to us so we can give you an appropriate response, either by reply-email or U.S Postal Service.
POSSIBLE CASE – Mitchell Thorp
Mitchell Thorp, a wonderful 16 year old boy, has grown up in Carlsbad, California with his mom Beth, his dad Brad, and his 14 year old brother Matthew.
In February 2004, the middle of Mitchell’s seventh grade year, he started experiencing severe headaches. After several attempts with different doctors nothing relieved his pain. Then, in September 2004, as Mitchell was starting his eighth grade year, it became increasingly difficult for him to concentrate.
Mitchell had always been a top student and very disciplined with his studies; but it became apparent the pain was so severe that Mitchell would have to continue his studies at home.
In October 2004, Mitchell was checked into Children’s Hospital for a complete workup. After three days of MRI scans, CT scans, extensive blood workup, and other tests, Mitchell and his parents left the hospital with no answers. The tests all came back negative/normal with no diagnosis made or cause found.
Mitchell was again admitted to San Diego Children’s Hospital in June 2005. And again he underwent MRI’s, lumbar punctures, blood workups, and a very complete series of tests. The neurologists, psychiatrists, hospital physicians, as well as others who were brought into this case, had no answers for what was happening to Mitchell. His appetite was decreasing at an alarming rate. He had lost 35 pounds and was now unable to either feed himself or walk.
In July 2005, shortly after leaving Children’s Hospital, Mitchell was admitted into the UCLA Pain Center. While there, Mitchell’s pain was so intense that the myoclonic seizures became constant and the tremors continuous. Mitchell spent most of his time unconscious because the pain was so severe. The doctor’s diagnosis is heavy metal toxicity coupled with a viral infection, which effects the central nervous system.
The goal now is to remove these metals from his body, so it can be restored to its original function. Mitchell is currently going through a number of therapies to achieve this goal. He has come a long way, but there is a long way to go.
He still cannot walk although he can get himself out of bed and scoot on the ground. He still cannot open his eyes, although it appears that one eye will lift half way. He still cannot speak. It is Mitchell’s hope, and the hope of all those around him that, as these metals are detoxed from his body, all of these functions will return.
NOTES: Since no other family member suffered from heavy metal toxicity, another source had to be found.
One fact that was noted that Mitch played a vigorous game of baseball immediately after the 2003 “Cedars Fire” ravaged San Diego. The smoke and debris was heavy in the air during the game.
This smoke and debris breathed, plus other factors unique to this young person at the time, could have been the “trigger” for his mysterious affliction. Mitch’ was treated a number of times at our San Diego Center and positive changes were noted. However, Mitch’s journey to recovery is continuing.
Join us in supporting the Thorp family as they have accumulated enormous medical expenses in trying to find a cure for their son.
Mitchell’s current and past medical expenses have reached heights far beyond the Thorp’s insurance coverage. Click here to to learn about Mitchell’s progress, where and how you can help.
Now the good news … Our HBOT centers have successfully treated and will treat chronic CO poisoning.
![]()

Clinical Example 1
A 40 year old physician was exposed to CO due to a faulty heater during a vacation. The night turned cold and she turned on the heater. Both parties woke with tahypnea (respiration rate > 40), tachycardia and headache.The physician fell when she tried to rise. She was between drowsy and stuporous and had to be assisted outside. She actually did quickly infer that it was CO poisoning based on the profile of symptoms and signs, with more than one party affected, and also information procured related to the heater (plus high CO levels found with purchase of a CO monitor); but she did not seek immediate care. (Some medical texts state there are no chronic sequelae of CO poisoning if there is not frank loss of consciousness.)
When still seriously impaired several days later she contacted a medical center and was advised treatment would be given if and only if COHb levels were still high. Because the reported half life of CO made this highly unlikely, she did not pursue this. After severe persistent symptoms at six months, she spoke to a University HBO physician who indicated that HBO was not an accepted treatment for chronic sequelae but only for acute toxicity (again, while CO levels were high). He indicated it would not be done at a University, but did suggest that it could be tried on the outside.
The physician then came to one of our Centers and was given 15 HBOT sessions at 2 ATA for 90 minutes. She felt normal after her treatments and returned to full time effective work. She has been followed up for over five years now and remains asymptomatic.
NOTES: It is important for others to know that there was *not* frank loss of consciousness but that chronic sequelae ensued nonetheless.
Equally important to note that, neurons have a long "shelf life" after chemical intoxication and, six months later it was possible to erase all negative symptoms and restore normal neuronal functioning.
Note that hospital HBOT specialists were not familiar with the fact that occult sequelae were ongoing, well after no COHb was detectable in blood tests and that rehabilitation was possible – not just spontaneous remission observed in acute CO poisoning.
Clinical Example 2
A 33 year old female lived for four years in an apartment with a faulty furnace. Over the years her behavior began to deteriorate with gross personality changes.Neurophysiological examinations revealed diffuse brain behavior involvement, with specific deficits in language, learning and recall of verbal material (short and long term memory) and positive features of depression. The faulty furnace was identified as a source of CO.
Since since no local hospital would treat her (her COHb were at "normal" levels also) the patient traveled from Philadelphia to the San Diego center for HBOT.
The patient received 30 HBOT sessions at 2 ATA for 90 minutes. She felt normal at the end of her treatments and returned home where her family and friends rejoiced at the "return of the girl we once knew".
She has been followed up for six years and remains asymptomatic.
1. “Carbon Monoxide: Identification of Delayed Sequelae and Occult Exposure” – J. Thomas Millington, M.D. Joel Ellenswig, M.D. Karen L Shiltz, PHD Hyperbaric Medicine Today, Volume II, Issue II, April – September 2003, pages 42–45.