High density oxygen (HBOT) not only acts as a potent bactericide, it also becomes a potent antifungal. Combined with the appropriate pharmaceuticals, toxic mold and fungus are rapidly eradicated from the body using multiple physiological mechanisms. We present a dramatic intervention that saved the life of this little person.
Miraculous recovery of six-year-old Carson C’
Carson was diagnosed with lymphoblastic leukemia and, while in the hospital, developed a severe opportunistic infection with dissementated mucormycosis during the induction phase of his chemotherapy.
This usually fatal infection is not uncommon in the severely immunosuppressed patients such as Carson. The infection is so rapid and lethal, the conventional medical response is an urgent mixture of surgery (debride until bleeding tissue is found) and antifungal agents.
In a ten-day period, Carson surgeon’s removed one kidney from Carson, his spleen and most of his colon. Plans were made to remove the little boy’s left lung and his stomach.
Staff at Children’ Hospital of San Diego did not believe that Carson would survive the surgery and at the urging of Carson’s mother, herself an M.D., they considered adding hypberbaric oxygen therapy (HBOT) for his survival. They consulted local San Diego hospital-based HBOT centers and were unable to treat Carson …
“Yes, this soft-tissue infection is covered by our guidelines. We would love to help but our wound care patients have us jammed for weeks …”
Children’s Hospital oncologist called our free standing HBOT Center. “Yes” was our answer.
“Although HBOT has been used all around the world to eradicated disseminated fungi such as mucormycosis for many years, using HBOT for mucormycosis is unusual in the U.S. … and yes, we have the skills to treat your patient, send him over.
“This is not the first time we have treated one of your little patients from Childrens’ “
(Read about Amci’s limb salvage on the Disease & Trauma to Bones page)
Children’s Hospital oncologists and surgeons immediately called for an in-house investigational review board (IRB) which reviewed the available literature. The IRB authorized outpatient treatment for Carson with full emergency-care ambulance transport to the Center. The little patient’s medical insurer reviewed the physician’s orders and approved treatments.
Result:
The mucor disappeared and Carson did not need additional desperate surgery. On a daily basis, Carson continues to regain weight and strength. Carson lives and will continue to do so. The Children’s Hospital primary oncologist for Carson wrote
“He has had a miraculous recovery with hyperbaric oxygen contributing to this response. This infection is usually fatal, yet Carson has survived and at present remains on chemotherapy.”
Dr. Tom Millington, World-renown HBOT specialist commented:
“Mucormycosis is on the list of approved conditions under the heading of certain anaerobic infections (actinomycosis, mucormycosis). Although mucormycosis is a condition which is approved for treatment, most facilities have never seen a case, and may be either uncomfortable treating a patient with this, or unaware that it can be treated.”
Summary:
HBOT is an adjunctive and supportive medical procedure for patients that are dramatically ill. This soft tissue necrotizing infection is one of the Undersea and Hyperbaric Society’s (UHMS) “approved list” for hospital treatment.
Nonetheless, since this is such an unusual and dramatic situation, the specialist physicians at Children’s Hospital are to be congratulated for their excellent medical opinion and their courage in stepping outside the “conventional” medical guidelines for this infection.
Medical information from Children’s Hospital *
Case Reports:
IRB approval and full signed informed consent (parent and child) was obtained regarding presentation of these case summaries. HIPAA guidelines were followed accordingly.
CASE 1:
The first child is a 6 year old male diagnosed with standard risk acute lymphoblastic leukemia (ALL) in September of 2006. The combination of newly diagnosed ALL with administration a three-drug induction including dexamethasone and resulted in profound neutropenia.
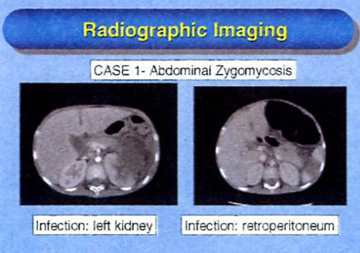
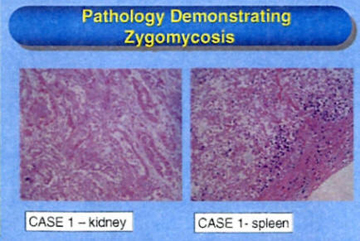
During the third week of chemotherapy, he developed zygomycosis in the left upper abdomen involving the colon, adrenal, left kidney, and pancreatic tail with suspected involvement of the retroperitoneum. The patient underwent left adrenalectomy, splenectomy, and left nephrectomy along with removal of the splenic flexure of the colon with diverting colostomy at the end of induction chemotherapy.
Diluted L-AMB also was diluted and irrigated into the abdomen at the time of this surgical procedure. The patient received L-AMB (10 mg/kg) with micufungin and GM-CSF. His neutrophil count recovered and he was confirmed as being in full morphologic and molecular remission at day 29 of therapy. Thoracotomy was performed to evaluate pleural effusion and consolidation but pathology was negative for zygomycosis.
He recently underwent surgical exploration of the abdomen and stomach along with colonic reanastomosis. No evidence of zygomycosis was found surgically or on review of pathology specimens after more than three months of antifungal therapy.
Hospital Conclusions
• The combination of liposomal amphotericin, micafungin, GM-CSF may be effective in treating zygomycosis in immunocompromised patients.
• Neutrophil recovery was essential for improvement in both patients.
• The role of hyperbaric oxygen remains to be evaluated but may have contributed to improvement in one patient.
• Neither patient had complete surgical debridement of all areas involved due to potential excessive morbidity; yet both are doing well clinically with medical therapy alone.
• Both patients require ongoing chemotherapy and will require close follow-up with collaboration between infectious disease and oncology teams.
![]()
* Extracts taken from “Successful Treatment of Zygomycosis with the Combination of Liposmal Amphotericin B, Micafungin and GM-CSF in Two Immunocompromised Children with Lymphoid Malignancies” – J willert, M Hilfiker, A Pong, J Leake, TJ Walsh, Rady Childrens Hospital San Diego, San Diego University of California, San Diego, NCI Bethesda, MD.
Notes from the Hyperbaric O2 Center
Patient Carson C’Six-year-old patient (Carson) was transported to San Diego Hyperbaric Center by Ambulance for his first HBOT treatment on 11/28/06. HBOT was ordered by specialist physicians as an adjunctive treatment modality for a fulminating mucor infection.
The Hyperbaric Chambers: An FDA Cleared chamber to accommodate a care-giver and the patient. The chamber is energized with 100% oxygen. No masks or hoods were used.
Based on the 1985 pioneering work of Professor Des Gorman, Head of the School of Medicine, Auckland New Zealand, in treating rhinocerebral mucormycosis plus the animal studies of Van Metre et al, a treatment pressure of 2.2 ata (18 psig) was selected. The hypothesis and in vitro studies showed the oxidative stress on fungus to be such that high density oxygen had a potent fungicidal effect. (http://www.medscape.com/viewarticle/432440_4)
Round One
Tx. 1 - 6 Special considerations for Carson:
LOADING: Carson had three major abdominal openings in previous eleven days and in considerable pain. He was weak and could not stand or crawl. The staff of the clinic devised a loading tray and Carson was transferred from his ambulance Gurney using a pull sheet. Carson then was transferred into the chamber from the tray using a pull sheet.
TREATMENT DEPTH: The specialist physicians had warned the staff that Carson had a large pleural effusion on his left side. No breath sounds could be heard and it was estimated that less than 10% vital lung function was available on that side. There was some contemplation that the zygomucor had invaded the entire L/H lung and that surgical removal of that lung was actually scheduled if he HBOT did not cause dramatic improvement.
The first sequential five days of Carson’s HBOT treatments consisted on low pressures, creeping upwards incrementally. This was to test the affected lung to ensure that no further damage would occur with the increasing pressure. Particular attention was paid for the decompression phase of each treatment to ensure that there was no gas entrapment in the lung.
Carson tolerated the treatments well and equalized his ears easily. For the first five days, the tympanic membrane was visualized and remained normal. Tympanostomy was not considered necessary.
After some of his early HBOT Tx, Carson was nauseous, “I am having a bad day.” This was in contrast with his pre-HBOT Tx posture of cheerful and good mentation. Since Carson was on parenteral nutrition, it was assumed that there was some degree of hypoglycemia. HBOT can produce dramatic drops in blood sugar levels in diabetic and pediatric patients.
Tx. 7 – 14 Treatment depth considerations for Carson:
Based on the hypoglycemia assumption and Carson’s post-Tx vomiting, the balance of the first series of Tx was reduced to 2 ata (14.7 psig.)
Carson’s strength had returned and he was more robust and regained strength. A decision was made to drain the pleural effusion and his first round of HBOT ceased for ten days.
Round Two
Tx 15 – Tx 31 Special considerations:
In view of the recent chest tap, a most conservative approach was taken to this treatment. The testing depth of 1.2 ata (2.67 psig) was selected. This to check visceral pleural integrity to ensure that there was no potential for a spontaneous pneumothorax. Such an event could result in a cerebral arterial gas embolism (CAGE.) Carson tolerated the Tx well and on the following day, his previous treatment depth of 2 ata (14.7 psig) was reintroduced.
Tx 32 - 33
With impending corrective surgery looming, Carson was treated at 2.2 Ata (18 psig.) The purpose of the increase was to blunt neutrophil mediated reperfusion injury without rendering the host functionally neutropenic and open to opportunistic infections. (Bartlet et al. See addendum)
Round Three
Tx 34
Five days after successful surgery, Carson commenced his third round of HBOT at 2.2 ata. (18 psig) The rational of this treatment pressure is that it accelerates wound healing, with large shifts in collagen production, fibroblasts and macrophage activity.
Go Carson – super kid!